54.
Dropsy of pregnancy: clinical signs, diagnostic, management and
prevention.
a form of the second half of pregnancy
toxemia, characterized by the appearance of edema in the absence of protein in
the urine and normal blood pressure.
Usually occurs after
28 to 30 weeks of pregnancy, often multiple.
Edema due to a
violation of water-salt metabolism and blood circulation in the capillaries and
the system as a result of the changed pre capillary neuro endocrine regulation.
A finding of new-onset
edema of the face and hands in association with proteinuria and elevated blood
pressure is consistent with preeclampsia.
Dependent pitting edema of the ankles and legs in the absence of
other findings is normal in late pregnancy.
It responds well to resting, with the legs elevated, and therefore
is usually absent on rising in the morning.
Sudden weight gain in the third trimester to a large extent
reflects an increase in edema.
Clinical sign-
excessive weight
gain per week (more than 250-400 g),
symptoms of "rings" (the ring on the
finger becomes stiffness),
"tight
shoes" (raznoshennaya shoes is close).
If measures are not
taken in a timely manner, there are visible swelling.
There are 4
prevalence of edema:
1)
only swelling in the
feet and lower legs,
2) edema of the
lower extremities, lower abdomen and lumbosacral region (if the woman is
lying), and 3) in addition to these, swelling of the hands, face pastosity
4 ) total edema.
The skin becomes
glossy look, keeping, however, the normal color (no pallor observed in renal
edema, cyanosis, as in edema associated with cardiac activity).
Even with pronounced
edema cardiac abnormalities, liver, kidney was observed.
There is no
accumulation of fluid in the well cavity (pleural and peritoneal).
During the rise of
edema observed decrease urine output (diuresis negative), reducing its share.
General state of the pregnant remains satisfactory.
Management-
Restriction of salt
(not more than 2g per day)
Reduce ammount of
fluid .
Analysis of blood
pressure ,urine,weight regularly.
Prescribe diuretics - gipotiazid (25
mg 2 times in the morning at four-hour intervals) 3 consecutive days,
for the night sedatives: motherwort
tincture at the rate of 10 g to 200 g of water on 1 table, HP, papaverine 0.02 g, better
in candles (for 1 suppository 2 times a day).
The woman should stay in bed (better defined
the diuretic effect).
Once a week, spend a day
of fasting (fluid restriction to 800 ml and salt to 2 g per day)
and after poluraspredelenia (without the first liquid dish).
Prescribe vitamins (vitamin C, vitamins of
group b). If within 3-4 days of improvement does not occur, then treated as if
nephropathy pregnant.
Diagnostic-
To check for edema that is not obvious, you can gently press your
thumb over the foot, ankle or leg with slow, steady pressure.
If edema is present, an
indentation will show on the skin. A
professional evaluation to determine the cause of leg swelling is needed.
If both legs are swollen,
your doctor will inquire about other symptoms and perform a physical examination.
A urine test will show whether you are losing protein from the
kidneys. Blood tests, a chest X-ray and
an electrocardiogram (ECG) may be ordered.
Prevention-
Careful monitoring and active patronage of pregnant women, monitor
their observance of hygiene, especially diet. Cm. also Pregnancy.
CHECK NUMBER 127
55.
Face presentation.
With this presentation, the head is hyperextended
so that the occiput is in contact with the fetal back, and the chin (mentum) is
presenting .
The fetal
face may present with the chin (mentum) anteriorly or posteriorly, relative to
the maternal symphysis pubis.
This position precludes flexion of the fetal head
necessary to negotiate the birth canal. Thus, a mentum posterior presentation
is undeliverable except with a very preterm fetus. Face presentations rarely
deliver as such vaginally.
.
Causes of
face presentations are numerous and include -
conditions that favor extension or prevent head
flexion.
Preterm infants, with their smaller head
dimensions, can engage before conversion to vertex position .
In exceptional instances, marked enlargement of
the neck or coils of cord around the neck may cause extension.
Diagnosis Face presentation-
diagnosed
by vaginal examination and palpation of facial features.
The
radiographic demonstration of the hyperextended head with the facial bones at
or below the pelvic inlet is characteristic.
Mechanism of Labor Face presentations
-
The mechanism of labor in these cases
consists of the cardinal movements of descent, internal rotation, and flexion,
and the accessory movements of extension and external rotation .
Descent is brought about by the same
factors as in cephalic presentations.
Extension results from the relation of the fetal body to the
deflected head, which is converted into a two-armed lever, the longer arm of
which extends from the occipital condyles to the occiput.
When resistance is encountered, the occiput must be pushed toward
the back of the fetus while the chin descends. The objective of internal
rotation of the face is to bring the chin under the symphysis pubis. Only in
this way can the neck traverse the posterior surface of the symphysis pubis.
If the chin rotates directly posteriorly, the relatively short
neck cannot span the anterior surface of the sacrum, which measures about 12 cm
in length. Moreover, the fetal brow (bregma) is pressed against the maternal
symphysis pubis.
This position precludes flexion necessary to negotiate the birth
canal. Hence, birth of the head from a mentum posterior position is impossible
unless the shoulders enter the pelvis at the same time, an event that is
impossible except when the fetus is extremely small or macerated. Internal
rotation results from the same factors as in vertex presentations.
After anterior rotation and descent, the chin and mouth appear at
the vulva, the undersurface of t he chin presses against the symphysis, and the
head is delivered by flexion. The nose, eyes, brow (bregma), and occiput then
appear in succession over the anterior margin of the perineum.
After birth of the head, the occiput sags backward toward the anus
Next, the chin rotates externally to the side toward which it was
originally directed, and the shoulders are born as in cephalic presentations.
Edema may sometimes significantly distort the face. At the same
time, the skull undergoes considerable molding, manifested by an increase in
length of the occipitomental diameter of the head.
Management
-In the absence of a
contracted pelvis, and with effective labor, successful vaginal delivery
usually will follow.
-Fetal heart rate monitoring
(is probably better done with external devices to avoid damage to
the face and eyes.)
-cesarean delivery frequently is indicated.
(Because face presentations among term-size fetuses are more
common when there is some degree of pelvic inlet contraction.)
56.
Preterm infants. Care and feeding of preterm infants.
what is preterm infants?-
Preterm infants is defined
as infants bron when labour occurring before 37 completed weeks.
It affects 5-10% of all pregnancies but it accounts for approximately 75% of
perinatal mortality.
Care and feeding of preterm infants-
The NICU is your newborn’s protective
environment and home for a limited period. Therefore, it is wise to become as
familiar with it as possible. The NICU
is equipped with caring staff, monitoring and alarm systems, respiratory and
resuscitation equipment, access to physicians in every pediatric specialty, 24
hour laboratory service.
monitors are similar in that they all record
heart rate, respiratory rate,blood pressure,
and temperature. A pulse oximeter may be used to measure the amount of oxygen
in the blood.
Gavage or tube feeding is used when infants are too smalll to
coordinate suck swallow and breathe.gavage may also be used to supplement
during or after breast feeding.
Cup feeding is also used to supplement breastfeeding in infants
with suck-swallow-breathe and gag reflex.
Breast feeding may be initiated when the infants is stable and can
gag.offer opportunities for non nutritive suckling before actual feeding.
57.
Cesarean section: indications and modifications of cesarean
section.
indications-
The four primary indications for cesarean
delivery include dystocia,
elective repeat cesarean delivery,
fetal distress,
abnormal fetal presentation.
The modification of cesarean section-
The delivery method of
choice is cesarean section, with the choice of uterine incision being dependent
on the placental location. A low transverse incision is selected if the lower
uterine segment is well developed. In many cases, however, the lower uterine
segment is poorly developed and a vertical incision is required.
All efforts should be made to avoid cutting through the placenta
during delivery, because this can be associated with massive maternal
hemorrhage and fetal blood loss. Blood loss can also be significant after
delivery of the placenta as a result of lower uterine segment atony. A blood
loss of 1500 mL or more at cesarean section for placenta previa is not
uncommon.
Transverse Incisions
With the Pfannenstiel incision, t he skin and subcutaneous tissue
are incised using a low, transverse, slightly curvilinear incision.
This is made at the level of the pubic hairline, which is
typically 3 cm above the superior border of the symphysis pubis.
The incision is extended somewhat beyond the lateral borders of
the rectus abdominis muscles. It should be of adequate width to accommodate
delivery—12 to 15 cm is typical.
Vertical Incision
An infraumbilical midline vertical incision begins 2 to 3 cm above
the superior margin of the symphysis and should be of sufficient length to
allow fetal delivery without difficulty. Therefore, its length should
correspond with t he estimated fetal size, and 12 to 15 cm is typical.
Low Transverse Cesarean Incision
Before any hysterotomy, the surgeon should palpate the fundus and
adnexa to identify degrees of uterine rotation. The uterus may be dextrorotated
so that the left round ligament is more anterior and closer to the midline.
In such cases, hysterotomy placement is modified to keep the
incision centered within the lower segment. This avoids extension into and
laceration of the left uterine artery.
58.
Craniotomy. Indications. Conditions. Techique.
What is craniotomy-
In case of obstructed labour with fetal death ,Reduction of the
size of the fetal head.
Indications and conditions
All the following conditions must hold:
(1)
The baby must be
dead.
(2) 2/5 or less of
his head must be above the brim (if it is higher than this, Caesarean section
is usually safer, although if you are expert you may be able to do it at 3/5).
(3)
His head must be
impacted.
(4)
His mother's cervix
must be at least 7 cm dilated, and preferably fully dilated. One contributor
gives 5 cm as the minimum.
(5) Her uterus must
be unruptured, and not in imminent danger of rupturing. If she is multigravid
and has been in labour for a long time, her lower segment will be very thin. If
it is tender and distended, it is certainly very thin. She can only be saved by
Caesarean section; any destructive operation, except pushing a needle into a
hydrocephalic head, will rupture it.
Techniques
Make a
cruciate (cross-shaped) incision on the scalp .
Cruciate incision
on scalp
Open the cranial vault at the lowest and most central bony point with a craniotome (or large pointed scissors or a heavy scalpel). In face presentation, perforate the orbits.
Insert
the craniotome into the fetal cranium and fragment the intracranial contents.
Grasp
the edges of the skull with several heavy-toothed forceps (e.g. Kocher’s) and
apply traction in the axis of the birth canal.
As the
head descends, pressure from the bony pelvis will cause the skull to collapse,
decreasing the cranial diameter.
If the head is not delivered easily, perform caesarean section.
After
delivery, examine the woman carefully and repair any tears to the cervix or vagina, or repair episiotomy.
Leave a
self-retaining catheter in place until it is confirmed that there is no bladder
injury.
Ensure
adequate fluid intake and urinary output.
59.
Transverse fetal positions (management of labor).
In this position, the long axis of
the fetus is approximately perpendicular to that of the mother. When the long
axis forms an acute angle, an oblique lie results.
In a transverse lie, the shoulder is usually
positioned over the pelvic inlet. The head occupies one iliac fossa, and the
breech the other.
This creates a shoulder presentation
in which the side of the mother on which the acromion rests determines the
designation of the lie as right or left acromial.
And because in either position the
back may be directed anteriorly or posteriorly, superiorly or inferiorly, it is
customary to distinguish varieties as dorsoanterior and dorsoposterior (Fig.
23-9)
management During transverse fetal
position
Active labor in a woman with a
transverse lie is usually an indication for cesarean delivery.
Before labor or early in labor, with
the membranes intact, attempts at external version are worthwhile in the
absence of other complications.
If the fetal head can be maneuvered
by abdominal manipulation into the pelvis, it should be held there during the
next several contractions in an attempt to fix the head in the pelvis.
With cesarean delivery, because
neither the feet nor the head of the fetus occupies the lower uterine segment,
a low transverse incision into the uterus may lead to difficult fetal
extraction.
This is especially true of
dorsoanterior presentations. Therefore, a vertical incision is typically
indicated.
60. Obstetrical assessment of the labor in vertex presentation.
61. Mechanism and purpose of obstetrical forceps.
Advantages to forceps use include
avoidance of C-section, reduction of delivery time, general applicability with
cephalic presentation. Complications include the possibility of bruising,
deformation, rectovaginal
fistula, nerve damage, Descemet's
membrane rupture (extraordinarily rare),skull fractures, and
cervical cord injury.
·
Maternal factors
1
Maternal exhaustion
2
Prolonged second
stage
3
Maternal illness;
such as heart disease, hypertension, glaucoma, aneurysm, or other things which
make pushing difficult or dangerous
4
Haemorrhage
5
Analgesic
drug-related inhibition of maternal effort (especially with epidural/spinal
anaesthesia)
·
Fetal Factors
6
Non-reassuring fetal
heart tracing
7
After-coming head in
breech delivery.
Mechanism
The way
the forceps are applied depends on the position and station of the baby's head,
the specific type of forceps to be used, and the experience and training of the
provider.
In
occiput anterior positions (baby facing down) the forceps blades should slide
easily into place along the doctor's hand that is in the vagina.
Usually
the left blade is inserted first (the left blade is defined as the blade that
goes between the baby's head and the left side of the mother's pelvis).
The
right blade is then inserted in the same fashion and the lock of the two blades
should come together easily.
Each blade should be about a finger's width
below the posterior fontanelle (the "soft spot" in the back of the
baby's head between the unfused cranial bones).
When
properly applied to a baby in occiput anterior position, the blades will extend
in front of the baby's ears and on to the cheeks.
When
the baby is in occiput posterior presentation (facing up), the blades can be
applied in the same fashion as for an occiput anterior (facing down)
presentation.
The
tips of the blades still rest on the baby's cheeks, but in this position the
blades meet just below the anterior fontanelle.
When
the baby's head is in a transverse position (facing the side of the pelvis),
the back blade is inserted first to help stabilize the position of the baby's
head.
Once
the forceps have been applied, it is important for the doctor to make sure they
are properly positioned on the baby's head.
If the forceps application is not easy or
requires force, then something isn't right. Commonly, this means that the
station is not as low as expected or that the position of the head has been
incorrectly assessed.
It may also mean that the wrong type of
forceps is being used. If the forceps don't go on easily, they shouldn't be
forced.
Rotation
and Traction
Once
properly applied, obstetric forceps can be used for rotation of the baby's head
and for traction for delivery of the head.
Rotation
An
outlet forceps delivery may be performed when the baby's head is visible at the
vaginal opening and is within 45 degrees of an occiput anterior or an occiput
posterior presentation. As the baby's head is rotated, traction is usually
simultaneously performed.
Rotations
greater than 45 degrees can safely be performed with forceps, but are
associated with a greater potential for complications.
Larger
rotations often require that the baby's station be shifted further up or
further down the birth canal. It is important that a very skilled and
experienced provider perform any of these more complicated maneuvers. A doctor
that has experience in manipulation of the forceps can utilize the pelvic curve
in the safest and most successful way possible.
Traction (Pulling)
Forceps
are most often used to apply traction to guide the baby down and out through
the birth canal. Traction should be directed along the axis of the birth
canal-that is, behind and under the pubic bone. With occiput anterior
presentations, this will often result in the handles of the forceps being
directed downward and then upward as the back of the baby's head comes under
the pubic bone. When a baby is being delivered in the occiput posterior
position, the traction will need to be directed downward.
Traction
should be applied in association with contractions and pushing efforts, with
rest periods in between. It is important to avoid undue pressure on the baby's
head; the doctor does this by loosening the handles in between contractions.
After
Delivery
Some
providers will remove the forceps before the baby is delivered and allow the
head to deliver spontaneously; others will remove the forceps after the baby's
head is delivered. There is no evidence proving that one approach is better
than the other. The decision, therefore, often depends on the potential urgency
of delivery. As with all deliveries, the condition of the baby should be
assessed immediately after delivery.
62.
Classification of contracted pelvis according to the form and
degree of contraction.
To anomalies of bone pelvis belong such anatomic
changes where all or one of external pelvic sizes is different from normal size
for 2cm. and more.
Classification-
63.
Spontaneous abortions. Causes. Management. Prevention.
termination of pregnancy by any means before the fetus is
sufficiently developed to survive (before 22 weeks).
Abortion is the most common complication of pregnancy. 10–15% of
all clinically recognised pregnancies end in a miscarriage. More than 80% of
abortions occur in 12weeks of gestation.
Causes-
Defective embryological development resulting from abnormal
chromosome division.
Faulty implantation of the fertilized ovum.
Failure of the endometrium to accept the fertilized ovum.
Premature separation of the normally implanted placenta
Abnormal placental implantation
Infection,severe malnutrition and abnormalities of the
reproductive organs.
Endocrine problems,such as thyroid dysfunction or a luteal phase
defect.
Trauma,including any surgery that requires manipulation of the
pelvic organs.
Phospholipid antibody disorder
Blood group incompatibility
Drug ingestion
Management-
Because of the risk of DIC (
disseminated intravascular coagulation)
with retained IUFD (Intrauterine fetal demise ), the best
treatment is delivery.
Early gestations can be evacuated from the uterus by dilation and
evacuation or with mifepristone and misoprostol in some cases.
After 20 weeks, the
pregnancy is usually terminated by induction of labor with prostaglandins or
high-dose oxytocin.
Helping patients understand what may have caused the fetal death
is imperative to helping them cope with the situation.
Tests for causes of fetal death include screening for collagen
vascular disease or hypercoagulable state, fetal karyotype, and often TORCH
titers (i.e., toxoplasmosis, RPR, CMV, and HSV). Because the cells of an IUFD
will often not grow to obtain karyotype, recent studies have examined
performing microarray studies of the fetal or placental genome to both look for
aneuploidy, in addition to, other genetic abnormalities such as copy number
variants.
It is also extremely important to get an autopsy on the fetus,
which can contribute valuable information. Despite this extensive battery of
tests, the etiology of fetal demise will likely remain unknown in the majority
of cases.
Prevention-
·
Encourage reduction
of alcohol consumption.
·
Smoking cessation
and stopping illicit drug use.
·
Intake of
nutritional natural food
·
Avoid of getting
pregnant before proper development of organs.
·
Avoid trauma risk.
·
Keep weight in limit
·
Regular exercise.
64.
Postpartum hemorrhages due to defective coagulaton (clinic,
diagnostic, management).
Postpartum hemorrhage is defined as blood loss in excess of 500 mL
at the time of vaginal delivery. There is normally a greater blood loss
following delivery by cesarean section; therefore, blood loss in excess of 1000
mL is considered a postpartum hemorrhage in such patients.
Most of the blood loss occurs from the myometrial spiral
arterioles and decidual veins that previously supplied and drained the
intervillous spaces of the placenta.
As the contractions of the partially empty uterus cause placental
separation, bleeding occurs and continues until the uterine musculature
contracts around the blood vessels and acts as a physiologic-anatomic ligature.
Failure of the uterus to contract after placental separation
(uterine atony) leads to excessive placental site bleeding.
Clinic-
Blood loss more than 1000ml
Blood pressure fall
Palpitation
Dizziness
Tachycardia
Presents of anemia
Diagnosis-
estimate how much blood lost.
Measuring pulse and the blood pressure
Red blood cells count
Count for clotting factors in blood
Management-
·
Medicine or uterine massage to
stimulate uterine contractions.
·
Removing pieces of the placenta that
remain in the uterus.
·
Exam of the uterus and other pelvic
tissues, the vagina, and the vulva to look for areas that may need repair.
·
Bakri balloon or a Foley catheter to
put pressure on the bleeding inside the uterus.
healthcare provider may pack the uterus with sponges and sterile
materials. This may be done if a Bakri balloon or Foley catheter is not available.
·
Laparotomy. This is surgery to open
the abdomen to find the cause of bleeding.
·
Tying off or sealing bleeding blood
vessels. This is done using uterine compression sutures, special gel, glue, or
coils. The surgery is done during a laparotomy.
·
Hysterectomy. This is surgery to
remove the uterus. In most cases, this is a last resort.
Replacing lost blood
and fluids is important in treating postpartum hemorrhage. may quickly be given IV (intravenous) fluids,
blood, and blood products to prevent shock. Oxygen may also help.
65.
Threatened rupture of perineum (clinic
and prevention).
All except the most
superficial perineal lacerations are accompanied by varying degrees of injury
to the lower portion of the vagina.
Such tears may reach sufficient depth to involve the
rectal sphincter and may extend to varying depths through the walls of the
vagina.
Bilateral lacerations into the vagina are usually unequal
in length and separated by a tongue-shaped portion of vaginal mucosa.
Clinic-
·
Failure of foal to
pass through vaginovestibular sphincter.
·
First-degree
laceration involving mucosa of vestibule and skin of dorsal commissure of
vulva.
·
Second-degree
laceration involving vestibular mucosa and submucosa, skin of dorsal commissure
of vulva and perineal muscles including constrictor vulva.
·
Rectovestibular
fistula involving ceiling of vestibule, floor of rectum, and variable amount of
perineal septum and musculature.
·
Third-degree
laceration involving ceiling of vestibule, rectal floor, perineal septum and
musculature, and anal sphincter.
Prevention-
66.
Generalized septic infection in puerperium.
Puerperal infections, also known as postpartum infections, puerperal
fever or childbed fever, is any
bacterial infection
of thefemale
reproductive tract following childbirth or miscarriage.
Signs and symptoms usually
include a fever greater than
38.0 °C (100.4 °F), chills, lower abdominal pain, and possibly bad-smelling vaginal discharge.[1]
It usually occurs after the first 24 hours and within the first ten days
following delivery.
The most common
infection is that of the uterus
and surrounding tissues known as puerperal
sepsis or postpartum metritis.
Causes and Risk
factors include-
woman's genital tract
has a large bare surface
septicaemia (blood
poisoning) or other illnesses
Generalized
peritonitis
Cellulitis
Other virulence
infections
the presence of
certain bacteria such as group B
streptococcus in the vagina,
multiple vaginal exams,
manual removal of
the placenta,
prolonged labour among
others.
Diagnosis- is rarely helped by culturing
of the vagina or blood. In those who do not improve medical imaging may be
required. Other causes of fever following delivery include: breast engorgement, urinary tract
infections, infections of the abdominal incision or episiotomy, and atelectasis.
Treatment-
C-section it is
recommended that all women receive a preventive dose of antibiotics such as ampicillinaround the time
of surgery.
Treatment of
established infections is with antibiotics, with most people improving in two
to three days. In those with mild disease oral antibiotics may be used
otherwise intravenous
antibiotics are recommended.
Common antibiotics
include a combination of ampicillin
and gentamicin following
vaginal delivery or clindamycin
and gentamicin in those who have had a C-section.
In those who are not
improving with appropriate treatment other complications such an abscess should be
considered.
67.
Course and management of the 3rd stage of labor.
3rd stage of labor
lasts from the birth of the baby until the placenta is expelled.
Physiological
process of placental seperation
Placental separation
Descend of the
placenta
Expulsion of
placenta
Delivery of the
Placenta Separation of the placenta generally occurs within 2 to 10 minutes of
the end of the second stage of labor.
Squeezing of the
fundus to hasten placental separation is not recommended because it may
increase the likelihood of passage of fetal cells into the maternal
circulation.
Mechanisms of
Placental Extrusion-
The retroplacental hematoma either follows the
placenta or is found within the inverted sac.
In this process,
known as the Schultze mechanism of placental expulsion, blood from the
placental site pours into the inverted
sac, not escaping externally until after extrusion of the placenta.
The other method of
placental extrusion is known as the Duncan mechanism.
in which separation of the placenta occurs
first at the periphery, with the result that blood collects between the
membranes and the uterine wall and escapes from the vagina.
In this
circumstance, the placenta descends to the vagina sideways, and the maternal
surface is the first to appear at the vulva.
Signs of placental
separation are as follows:
(1)
a fresh show of
blood from the vagina,
(2)
the umbilical cord
lengthens outside the vagina,
(3)
the fundus of the
uterus rises up, and
(4)
the uterus becomes
firm and globular.
Traction on the
umbilical cord must not be used to pull the placenta out of the uterus. Only
when these signs have appeared should the assistant attempt traction on the
cord.
With gentle traction
and counterpressure between the symphysis and fundus to prevent descent of the
uterus into the pelvis, the placenta is delivered.
Following delivery
of the placenta, attention should be paid to any uterine bleeding that may
originate from the placental implantation site.
Uterine
contractions, which reduce this bleeding, may be hastened by uterine massage
and the use of oxytocin.
It is routine to add
20 units of oxytocin to the intravenous infusion after the baby has been
delivered.
The placenta should
be examined to ensure its
complete removal and
to detect placental abnormalities.
If the patient is at
risk of postpartum hemorrhage (e.g., because of anemia, prolonged oxytocic
augmentation of labor, multiple gestation, or hydramnios), manual removal of
the placenta, manual exploration of the uterus, or both may be necessary.
68.
Mechanism of placental separation.
2 type of mechanism
1- Schultze mechanism of placental expulsion
2-duncan mechanism
In schultze mechanism
The retroplacental hematoma either follows the placenta or is
found within the inverted sac.
blood from the
placental site pours into the inverted
sac, not escaping externally until after extrusion of the placenta.
Duncan mechanism-
in which separation of the placenta occurs first at the periphery,
with the result that blood collects between the membranes and the uterine wall
and escapes from the vagina.
In this circumstance, the
placenta descends to the vagina sideways, and the maternal surface is the first
to appear at the vulva.
Signs of placental
separation are as follows:
(1)
a fresh show of blood from the vagina,
(2)
the umbilical cord lengthens outside the vagina,
(3)
the fundus of the uterus rises up, and
(4)
the uterus becomes firm and globular.
69.
Management of perineal incisions.
Laceration should be repaired immediately if possible,and certain
within 24 hours of delivery.
First step is to define the limits of the lacerations,which
includes vagina as well as perineum.
Best suture material is catgut for the vagina and buried sutures
and fine mono-filament nlon for skin.
As accurate an approximation as possible of all the tissues should
be secured and no dead spaces are left.
The after-care of the repaired perineal injures
is similar to that following episiotomy. Special care following repair of
complete tear.
1. A low residual diet consisting of milk, bread, egg, fish is given from
2nd day onwards.
2. Lactulose 8 ml twice daily beginning on the second day and increasing
the dose to 15 ml on the third day is a satisfactory regime to soften the
stool.
3. Any one
of the broad spectrum antibiotics is used during the intraoperative and the
post-operative period
70.
Nephropathy of pregnancy. Clinic and management.
71.
Course and management in puerperium.
Check question no 117
72.
Ruptures of vagina and perineum.Etiology, prevention,
management.
Etiology-
Vaginal-
During vaginal delivery, lacerations of the cervix and vagina may
occur spontaneously (fetal mal presentation,insufficient distensibility of
vaginal wall,large featl head), but they are more common following the use of
forceps or a vacuum extractor.
The vascular beds in the genital tract are engorged during
pregnancy, and bleeding can be profuse.
Lacerations are particularly prone to occur over the perineal
body, in the periurethral area, and over the ischial spines along the
posterolateral aspects of the vagina.
Vaginal laceration usually longitudinal
The cervix may lacerate at the two lateral angles while rapidly
dilating in the first stage of labor.
Management of vaginal laceration-
Tears associated with brisk haemorrage, require exploration under
general anaesthesia with good light.
The tears are repaired by interrupted or continuous sutures using
catgut.
In case of extensive lacerations, in additions to sutures,
haemostasis may be achieved by intravaginal plugging by roller gauze, soaked
with glycerine.
The plug should be removed after 24 hours.
Prevention-
exercise by
contacting, holding and then releasing the pelvic muscles. It can be easily
performed in a manner as trying to consciously hold the urine.
Regular kegel
exercises and other pelvic training activities help in strengthening the pelvic
muscles.
Maintaining healthy
consumption of fibrous fruits and vegetables along with adequate amounts of
water helps in improving the skin elasticity.
An elastic skin is
more resistant to tearing and rupture under pressure and stress.
After 34th week of
pregnancy, perineal massage should be regularly performed by applying a
lubricating gel on the perineum and then gentle rubbing.
Perineum-
Over stretching of the
perineum due to large baby, face-to-pubis or face delivery, outlet contraction
with narrow pubic arch, shoulder delivery (posterior one) and forceps
delivery.
Rapid stretching of the perineum due to rapid delivery of the head
during uterine contraction, precipitate labour and delivery of the after-coming
head in breech.
Inelastic perineum as in rigid perineum in elderly primigravidae,
scar in the perineum following previous operations such as episiotomy or
perineorrhaphy and vulval oedema.
DEGREES.
First degree : Involves lacerations of the remnants of the hymen,
the fourchette, lower part of the vagina and the perineal skin but the perineal
body remains intact.
Second degree : Involves
lacerations of the posterior vaginal wall and varying degrees of tear of the
perineal body excluding the anal sphincter.
Third degree : Injury of the perineum involving posterior vaginal
wall and tear of the perineal body including the anal sphincter complex with or
without involvement of the anal canal or even the rectum.
MANAGEMENT. Repair of complete perineal tear.
Look question no 69 for perineal management.
Prevention-
Perineal massage is reduce the risk of trauma.
Water birth and laboring in water will make the perineum soft and
reduce tearing.
Avoid pushing when baby crowning.
Take nutritional food
Use lubricants
73. Causes of uterine bleedings after child delivery.
After the baby is
delivered, excessive bleeding from the uterus is a major concern. Ordinarily,
the woman loses about 1 pint of blood after vaginal delivery.
Blood is lost
because some blood vessels are opened when the placenta detaches from the
uterus. The contractions of the uterus help close these vessels until the
vessels can heal.
Typically, cesarean
delivery results in about twice the blood loss as vaginal delivery, partly
because delivery requires an incision in the uterus, and a lot of blood is
pumped to the uterus during labor.
Excessive bleeding
may result when the contractions of the uterus after delivery are impaired.
Then, the blood
vessels that were opened when the placenta detached continue to bleed.
Contractions may be impaired in the following situations.
Overdistention of the uterus
Mulliple gestation
Polyhydramnios
Fetal microsomia
Prolonged labor
Oxytocin augmentation of labor
Grand multi parity (a parity of 5 or more)
Precipitous labor (one lasting -<3 hr)
Magnesium sulfate treatment of pre-eclampsia Chonoamnionilis
Halogenated anesthetics
Uterine leiomyomata.
74.Multiple
pregnancy. Clinic and diagnostic. Management of labor.
clinical science-
Increased nausea and vomiting in early months.
Cardio respiratory embarrassment
Tendency and swelling in legs,varicose vein and hemorrhoids is
greater
Unusual rate uterine enlargement and excessive fetal movements.
Diagnostic-
Family history for multiple pregnancy.
Increased fetal movement.
More enlargement of abdomen.
Fundal level higher than normal
Fetal heart sound heard with maximum intensity in 2 separate
points by 2 observers with a minimum different of 10 beats per minutes.
Occasionally the superimposition of two fetal heart sound produces
a galloping rhythm.
Ultrasonography - separate gastation sacs can be identified.in 7th
week
Separated fetal bodies can
be detected in 8th week.
Separated heads can be detected in 12th week
X-ray -
It can detect fetal heads and fetal columns.
Management during labor-
Delivery should be in hospital
A team of experienced obstetrician,assistant,anaesthetist and
neonatologist is necessary for safety.
Delivery of the first fetal, if it is cephalic proceed as
normal,if it is breech cesarean section is safe,although vaginal delivery may
pass without complication.
Immediate clamping of the cord is essential after delivery of the
first fetal to avoid bleeding from a second fetal.
Delivery of th esecond fetus, it depends upon its
presentation,longitudinal lie, transverse or oblique lie.
75.
Urogenital and intestinal fistulas. Etiology and prevention.
Etiology-
Prevention-
Rupture uterus
/emergency obstetrical
Hysterectomy.
Post operative
period.
76.
Abnormal uterine action.
ETIOLOGY.
As the physiology of normal uterine contraction is not fully
understood, the cause of its disordered action remain obscure. However, the
following clinical conditions are often associated:
1.
prevalent in first birth specially with advancing age of the
mother;
2.
prolong pregnancy;
3.
over distension of the uterus due to twins and/or hydramnios;
4.
psychologic factor;
5.
contracted pelvis, malpresentation and deflexed head, full bladder
are often associated too; all this lead to ill fitting of the presenting part
into the lower uterine segment; this probably result in inhibition of the local
reflex which is needed to produce effective contraction of the upper segment;
6.
injudicious administration of sedatives, analgesics and oxytocics;
7.
premature attempt at vaginal delivery.
The uterine pace maker is situated at the cornua of the uterus and
this generates uterine contractions Effective uterine contraction, starts at
the cornua and gradually sweep downwards over the uterus.
In a primary dysfunctional labour, uterine activity instead of
being governed by a single dominant space maker, is shifted to less efficient
contractions due to emergence of other pacemaker foci.
2). Oxytocin therapy may be effective in restoring the global and
effective uterine contractions.
Primary dysfunctional labour
is defined when the cervix dilates < 1 cm/hr. It is a commonest abnormality
and mostly corrected by amniotomy and/or oxytocin augmentation.
Secondary arrest is defined when the cervical dilatation stops or
slows after the active phase of labour has started normally.
Uterine activity (contraction) is measured by noting basal tone,
active (peak) pressure and frequency. Assessment is usually done by:
1.
clinical palpation (inaccurate);
2.tocodynamometer
with external transducer;
3.
using intrauterine pressure catheter (accurate). Normal baseline
tonus is between 5 and 20 mm of Hg and peak pressure is around 60 mm of Hg (8
Kpa).
Uterine inertia (hypotonic activity) Uterine inertia is the common
type of disordered uterine contraction but is comparatively less serious. It
may complicate any stage of labour. It may be present from the beginning of
labour or may develop subsequently after a variable period of effective
contractions.
The intensity of uterine contractions is diminished, duration is
shortened, good relaxation in between contractions and the intervals are
increased. General pattern of uterine contractions of labour is maintained but
intrauterine pressure during contraction hardly rises above 25 mm of Hg.
Diagnosis:
patient feels less pain
during uterine contraction; hand placed over the uterus during uterine
contraction reveals less hardening of the uterus; uterine wall is easily
indentable at the acme of
the pain; uterus becomes relaxed after the contraction; fetal
parts are well palpable and fetal heart rate remains good.
Internal examination
reveals poor dilatations of the cervix (normal rate of dilatation in
primigravida should be at the rate of 1 cm per hour beyond 3 cm dilatation),
associated presence of contracted pelvis, malposition, deflexed head or
malpresentation may be evident; membranes usually remains intact. It’s
necessary to exclude cephalopelvic disproportion or malpresentation. In a case
of contracted pelvis, malpresentation or fetal distress cesarean section is
indicated.
In other cases we should propose active measures – acceleration of
uterine contraction can be brought about by low rupture of the membranes
followed by oxytocin or prostaglandins drip.
The drip rate is gradually increased until effective contraction
are set up. The drip is to be continued till one hour after delivery. If the
cervical dilatation remains unsatisfactory and/or fetal distress appears,
caesarean section is the best alternative.
77.
Face presentation. Mechanism of labor and management.
check question no -55
78.
Uterine atony and postpartum hemorrhage.
The majority of postpartum hemorrhages (75% to 80%) are due to
uterine atony.
Factors Predisposing to Postpartum Uterine Atony Overdistention
of the uterus
Mulliple gestation
Polyhydramnios
Fetal microsomia
Prolonged labor
Oxytocin augmentation of labor
Grand multi parity (a parity of 5 or more)
Precipitous labor (one lasting -<3 hr)
Magnesium sulfate treatment of pre-eclampsia Chonoamnionilis
Halogenated anesthetics
Uterine leiomyomata.
If uterine atony is determined to be the cause of the postpartum
hemorrhage, a rapid continuous intravenous infusion of dilute oxytocin (40 to
80 U in 1 L of normal saline) should be given to increase uterine tone.
If the uterus remains atonic and the placental site bleeding
continues during the oxytocin infusion, ergonovine maleate or methylergonovine,
methylergometrine.
Analogues of prostaglandin F2α given intramuscularly are quite
effective in controlling postpartum hemorrhage caused by uterine atony.
Failing these pharmacologic treatments, a bimanual compression and
massage of the uterine corpus may control the bleeding and cause the uterus to
contract.
Although packing the uterine cavity is not widely practiced, it
may occasionally control postpartum hemorrhage and obviate the need for
surgical intervention
The vital signs, hematocrit, and fundal height should be monitored
frequently while the packing is in place, because continued bleeding will not
be initially evident through the packing.
The packing may be removed in 1 to 4 hours. Usually, the bleeding
will be controlled.
Another approach that may
be tried if bleeding persists is placement of the patient into an antigravity
suit (G suit), which will, when inflated, compress the lower extremities and
the abdominal cavity.
Experience with this device in trauma patients has demonstrated
good control of intra-abdominal bleeding. This approach may occasionally be
used temporarily while the blood volume is being expanded and preparations are
made for more definitive surgery. Operative intervention is a last resort. If
the patient has completed her childbearing, a supracervical abdominal
hysterectomy is definitive therapv for intractable postpartum hemorrhage caused
by uterine atony.
If reproductive potential is important to the patient, ligation of
the uterine arteries adjacent to the uterus will lower the pulse pressure
distal to the ligatures.
This procedure is more successful in controlling uterine placental
site hemorrhage and is easier to perform than bilateral hypogastric arterv
ligation.
79.
Prenatal care in maternity hospital.
Read the lecture topic prenatal.
80.
Extraction of fetus on breech delivery.
81. Obstetric forceps. Conditions, indications, technique of
operations.
Indications-
-Delay to uterine inertia
-Failure of orogress of labor-if no
progress occur more than 20 -30 min,with
the head on the perineum.
-Fetal distress in second stage when
prospect of vaginal delivery is safe-abnormal heart rate pattern
Passage of meconium
Abnormal scalp blood ph
-cord prolapse in second stage
-low birth wt.baby
-post maturity
Maternal indications
-pre eclampsia
-post cesarean pregnancy
-heart disease
- intra partum infection
-neurological disorder where
voluntary efforts are contraindicated or impossible
condition-
Cervix must be fully ruptured
Membranes must be ruptured
Baby should be living
Uterus should be contracting and
relaxing
Bladder must be empty
Technique -
82.
Technique of manual removal of afterbirth.
Separation of the placenta generally occurs within 2 to 10
minutes of the end of the second stage
of labor. Squeezing of the fundus to hasten placental separation is not
recommended because it may increase the likelihood of passage of fetal cells
into the maternal circulation.
Two types of techniques are there-
1- Schultze mechanism of placental expulsion.
The retroplacental hematoma either follows the placenta or is
found within the inverted sac. In this process,blood from the placental site pours into the inverted sac, not
escaping externally until after extrusion of the placenta.
2- Duncan mechanism
in which separation of the
placenta occurs first at the periphery, with the result that blood collects
between the membranes and the uterine wall and escapes from the vagina. In this
circumstance, the placenta descends to the vagina sideways, and the maternal
surface is the first to appear at the vulva.
83.
Puerperal parametritis and thrombophlebitis.
puerperal parametritis-
Causes-
Compared with cesarean delivery,
metritis following vaginal delivery is relatively infrequent.
Vaginal delivery-because of membrane
rupture, prolonged labor, and multiple cervical examinations
removal of the placenta.
Cesarean delivery-
surgery included prolonged labor, membrane
rupture, multiple cervical examinations, and internal fetal monitoring.
Abortion through placental site or
from laceration of cervix.
Diagnostic and clinical signs-
Fever is the most important criterion
for the diagnosis of postpartum metritis. Intuitively, the degree of fever is
believed proportional to the extent of infection and sepsis syndrome.
Temperatures commonly are 38 to 39°C. Chills that accompany fever suggest
bacteremia or endotoxemia.
Women usually complain of abdominal
pain, and parametrial tenderness is elicited on abdominal and bimanual
examination.
Leukocytosis may range from 15,000 to 30,000
cells/μL, but recall that cesarean delivery itself increases the leukocyte
count (Hartmann, 2000). Although an offensive odor may develop, many women have
foul-smelling lochia without evidence for infection, and vice versa.
Some other infections, notably those
caused by group A β-hemolytic streptococci, may be associated with scant,
odorless lochia.
Treatment-
treatment with an oral antimicrobial
agent is usually sufficient
For moderate to severe infections,
however, intravenous therapy with a broad-spectrum antimicrobial regimen is
indicated.
Thrombophlebitis -
It is a venous inflammation with
thrombus formation in association with fevers unresponsive to antibiotic
therapy.
Bacterial infection of the
endometrium seeds organisms into the venous circulation,which damages the
vascular endothelium and in turn result in thrombus formation.
The thrombus acts as a suitable
medium for proliferation of anaerobic bacteria.
Diagnostic-
History, it is usually accompanies
endometritis. Lower abdominal pain with or without radiation to the flank,groin
or upper abdomen.
Physical
examination,fever,tachycardia, on abdominal examination tender,palpable
ropelike mass.
Use CT and MRI scan.
84.
Premature rupture of amniotic fluid sac (causes, complications
for women and fetus).
This term defines spontaneous rupture of the fetal membranes
before 37 completed weeks and before labor onset.
Cervical incompetence,polyhydraminos,multiple
pregnancy,malpresentations as the presenting part is not fitting against the
lower uterine segment.
Chorioamnionitis
Low tensile strength of the membranes.
Causes-
Such rupture likely has various causes, but intrauterine infection
is believed by many to be a major predisposing event .
There are associated risk
factors that include low socioeconomic status, body mass index ≤ 19.8,
nutritional deficiencies, and cigarette smoking.
Complications-
For women-
Sepsis,placental abruption.
For fetus-
Chorioamnionitis,cord prolapse,PTL,pulmonary hypoplasia,limb
contractures,death.
85.
Diagnostic and management of missed miscarriage.
diagnostic-
Urine pregnancy test
FBC-full blood count
Blood group and GSH - to check rhesus ststus,and to prepare for
tranfusion
Ultrasound-locate the fetus,to assess viability and to look for
POC.
Histology-any tissues expelled should be investigated to exclude
molar or ectopic pregnancy.
Management-
Bed rest-
Progestagen-
86.
Assessment of fetal well-being
electronic fetal monitoring was used in 84% of all births,
regardless of whether the primary caregiver was a physician or a midwife. With
the advent of these technologies, fetal monitoring is implemented in nearly all
pregnancies, either in the antepartum or intrapartum period.
The goal is to prevent
fetal and neonatal morbidity and especially mortality.
Interpretation of the Fetal Monitor Tracing-
Analysis of the fetal
monitor strip requires a systematic approach. First, the FHR is analyzed with
respect to the baseline, variability, and periodic patterns, including FHR
accelerations and decelerations.
Baseline Fetal Heart Rate-The normal FHR baseline ranges from 120
to 160 beats per minute. Early in pregnancy, it is closer to 160 beats per
minute, declining as gestational age advances.
Likewise, the FHR may decrease gradually toward 120 beats per
minute during the course of labor. An FHR baseline below 120 beats per minute
is termed bradycardia, and a rate in excess of 160 beats per minute is termed
tachycardia.
Abnormalities in the FHR baseline may have very different causes
and consequences. It is important, therefore, to characterize the underlying
etiology as accurately as possible.
Bradycardia-
Bradycardia is defined as an abnormally low baseline FHR (<120
beats per minute). Although FHR decelerations are very common, true fetal
bradycardia is not. Rarely, fetal bradycardia may be seen in association with
maternal hypothermiahypoglycemia, hypothyroidism, or fetal cardiac conduction
defects (congenital atrioventricular block).
Documentation of fetal heart block should prompt a search for
structural fetal cardiac abnormalities, which may be present in 20% of cases.
Other causes of heart block include viral infections (e.g., cytomegalovirus)
and damage to the cardiac conduction system by transplacental passage of
maternal antiRo (anti-SS-A) antibodies. Most congenital causes of fetal
bradycardia do not present as abrupt changes in the FHR and rarely require emergency
intervention.
Any abrupt decline in the FHR below 120 beats per minute more
likely represents a deceleration than a change in the baseline.
Tachycardia-
Fetal tachycardia has many
possible etiologies. Most often, it is the result of decreased vagal or
increased sympathetic outflow, associated with fever, infection, fetal anemia,
or fetal hypoxia. Other causes include maternal hyperthyroidism, fetal
tachyarrhythmias (e.g., paroxysmal supraventricular tachycardia, atrial
fibrillation, atrial flutter, and ventricular tachyarrhythmias), and
medications ritodrine and atropine.
Sinusoidal Pattern-
The sinusoidal FHR pattern is an uncommon FHR baseline
abnormality. It has the appearance of a smooth sine wave with an amplitude of 5
to 15 beats per minute and a frequency of 2 to 5 cycles per minute. There is
little beat-to-beat variability, and accelerations are absent. Although the
pathophysiologic mechanism is unclear, this pattern classically is associated
with hypoxia and severe fetal anemia. Additionally, it has been reported in
association with chorioamnionitis, fetal sepsis, and administration of narcotic
analgesics.
Accelerations-
Accelerations in the FHR
occur with 90% of fetal movements as early as the second trimester, probably as
a result of increased catecholamine release and decreased vagal stimulation of
the heart. By 32 weeks gestation, nearly all normal fetuses will have 15 to 40
spontaneous accelerations per hour, reflecting normal oxygenation of the CNS
cardiac axis. The frequency and amplitude of accelerations may be diminished by
fetal sleep states, medications (narcotics, magnesium sulfate, atropine),
prematurity, or fetal acidosis. Often, fetal scalp stimulation or vibroacoustic
stimulation will provoke fetal movement and FHR accelerations. If these
measures fail to induce FHR accelerations, hypoxia should be suspected.
Decelerations-
Decelerations in the FHR
are most commonly
encountered during the intrapartum period. They are divided into
three categories: early, variable, and late decelerations. Classification is
based on the characteristic appearance of the deceleration and its temporal
relationship to the onset of a uterine contraction.
Early decelerations are
typically uniform, shallow dips in the FHR (rarely below 100 beats per minute)
that mirror uterine contractions, beginning at the onset of the contraction and
ending when the contraction ends. They are thought to result from fetal head
compression, transient elevation of intracranial pressure, and reflex augmentation
of vagal tone.
Early decelerations classically appear during labor when the
cervix is dilated 4 to 6 cm. Perinatal outcome is not adversely affected by
these decelerations, and they are considered clinically benign. Variable
decelerations result from umbilical cord compression.
They are abrupt and angular in appearance and have a variable
temporal relationship to uterine contractions. Variable decelerations are
classified as mild, moderate and severe. Isolated, infrequent variable
decelerations have little clinical significance. Repetitive severe variables,
however, may not allow sufficient fetal recovery between decelerations,
resulting in persistent hypoxemia, hypercapnia, and respiratory acidosis.
Prolonged tissue hypoperfusion may lead to metabolic acidosis and,
ultimately, fetal death. When repetitive, severe variable decelerations are
present, prolapse of the umbilical cord must be excluded. Other causes include
nuchal cord, true knot in the cord, uterine rupture, placental abruption,
uterine hypertonus, and tachysystole. Occasionally, variable decelerations fail
to return promptly to the baseline and may more accurately be called prolonged
decelerations.
Late decelerations reflect
inadequate uteroplacental transfer of oxygen during contractions. Typically,
they are smooth, uniform decelerations that begin after the onset of a
contraction and end after the contraction stops. Late decelerations may be
caused by any factor that reduces the normal placental transfer of oxygen or
increases the fetal oxygen demand beyond the available supply.
Such factors include uterine hypertonus or tachysystole (oxytocin,
prostaglandins, uterine rupture, placental abruption), maternal hypertension
(chronic hypertension, preeclampsia, collagen vascular disease, renal disease,
diabetes), suboptimal maternal cardiac output (cardiac disease, hypovolemia,
supine hypotension, sympathetic blockade from regional anesthesia, sepsis),
maternal hypoxia (apnea, cardiac disease, pulmonary disease), reduced
oxygen-carrying capacity of maternal blood (anemia, hemoglobinopathy), and
fever (increased fetal metabolism and increased oxygen consumption).
Biophysical Profile-
The BPP assesses five
variables: FHR reactivity, fetal movement, tone, and breathing (reflecting
acute CNS function), and amniotic fluid volume.
The volume of amniotic fluid is a measure of fetal well-being. By
the second trimester, the predominant source of amniotic fluid is fetal urine.
The level of amniotic fluid is thought to represent long-term fetal well-being.
A compromised fetus will preferentially shunt blood to the major
organs, such as the central nervous system (CNS) and adrenals, and away from
others, such as the kidney. Decreased fetal renal perfusion results in a
decrease in fetal renal function and subsequent oligohydramnios.
The amniotic fluid can be assessed ultrasonographically. Two
points are assigned for each normal variable and 0 for each abnormal variable
for a maximum score of 10. A BPP score of 8 to 10, with normal amniotic fluid
volume, is considered normal.
A score of 6 is considered suspicious, and testing usually is
repeated the following day. Scores of less than 6 are associated with increased
perinatal morbidity and mortality; they usually warrant hospitalization for
further evaluation or delivery. The BPP is a reliable predictor of fetal
well-being. Advantages of the BPP include excellent sensitivity, a weekly
testing interval, and a low false-negative rate. The primary limitation is the
requirement for personnel trained in sonography.
Additionally, although the duration of ultrasound observation is
typically less than 10 minutes, the complete BPP is more timeconsuming than
other noninvasive tests.
Doppler Velocimetry-
Doppler velocimetry of
fetal, umbilical, and uterine vessels has been the focus of intensive study in
recent years. This technology uses systolic-to-diastolic flow ratios and
resistance indices to estimate blood flow in various arteries.
Studies have shown significant improvement in perinatal outcome
with the use of Doppler ultrasonography in pregnancies complicated by growth
restriction.
Although severe restriction of umbilical artery blood flow, as
evidenced by absent or reversed flow during diastole, has been correlated with
fetal growth restriction, acidosis, and adverse perinatal outcome, the
predictive values of less extreme deviations from normal remain undefined.
In conditions other than
fetal growth restriction,
Doppler velocimetry does not appear to be a useful screening test
for the detection of fetal compromise and is not recommended for use as a
screening test in the general obstetric population.
Doppler velocimetry is used
in some settings as an adjunct to standard methods of fetal assessment but
should not be considered a replacement for traditional fetal monitoring.
Fetal Scalp Blood Sampling -
allows for the determination of the fetal acid-base status during
labor. The technique requires dilation of the cervix, rupture of the membranes,
and access to the fetal presenting part.
Since respiratory acidemia is generated in the blood and metabolic
acidemia is generated in the tissues, a scalp sample may not reflect the state
of the fetus.
In light of the technical difficulty of the procedure and the
uncertainty regarding interpretation of results, many centers have reduced
their reliance on fetal scalp blood sampling.
Percutaneous Umbilical Blood Sampling-
Electronic FHR monitoring,
ultrasound, and fetal scalp blood sampling can provide useful information
regarding the acid-base status of the fetus.
Occasionally, however, direct access to circulating fetal blood is
necessary. A classic example is the fetus with severe anemia secondary to Rh
isoimmunization.
63 Doppler studies of the middle cerebral artery are a noninvasive
method for the assessment of fetal anemia. In some cases, direct sampling of
the fetal blood and intrauterine blood transfusion may be required.
Percutaneous umbilical blood sampling (PUBS) is a procedure that
affords direct access to fetal venous blood.
Medications or blood may be infused through the needle once fetal
blood samples have been obtained. Other indications for PUBS include suspected
antibody-mediated fetal thrombocytopenia and fetal cardiac arrhythmias
requiring assessment of fetal drug levels or direct fetal administration of
antiarrhythmic agents.
87.
Pelvis justo minor. Mechanism of labor. Management of labor.
mechanism of labor-
88.
Third-trimester bleeding.
Vaginal bleeding in the third trimester complicates 4% of all
pregnancies.
It is considered an obstetric emergency because hemorrhage remains
the most frequent cause of maternal death.
It is critical for the well-being of both the mother and fetus
that the patient who presents with third-trimester bleeding be managed
expediently.
Causes of Antepartum Bleeding
Common
Placenta previa Abruptio
placentae
Uncommon
Uterine rupture
Fetal (chorionic) vessel rupture
Cervical or vaginal lacerations
Cervical or vaginal lesions including cancer Congenital bleeding
disorder
Unknown of the bleeding
Physical Examination -
The vital signs and amount of bleeding should be checked
immediately as should the patient's mental status. Whether the skin is moist or
dry and pale or mottled should be noted, as should the presence of petechial
hemorrhages or bleeding from any site other than the vagina, such as the nose
or rectum.
The abdominal examination
must include fundal height measurement and assessment of uterine tenderness. A
pelvic examination should not be performed until placenta previa has been
excluded by ultrasonography.
Investigations -
1-Laboratory Tests A complete blood count
should be obtained and compared with previous evaluations to help
assess the amount of blood loss. An assessment of the patient's coagulation
profile should be done by obtaining a platelet count, serum fibrinogen level,
prothrombin time, and partial thromboplastin time- it is often helpful to do a
"wall clot" test, whereby a red-topped tube of blood is drawn, taped
to the wall, and timed for clot formation. If no clot develops within 6
minutes, coagulopathy is most likely present. The patient should be typed and
crossmatched for at least 4 units of blood (packed cells).
2-Ultrasonography
The ultrasonographic evaluation should include not only the
location and character of the placenta, but also an assessment of gestational
age, an estimate of fetal weight, determination of the fetal presentation, and
a screening for fetal anomalies.
3-Monitoring
Uterine activity and the fetal heart rate should be assessed with
a monitored strip to rule out labor and establish fetal well-being.
Management-
89.
Signs of clinically contracted pelvis. Management of labor.
Clinical signs-
During pregnancy-
incarcerationof gravid uterus into pelvis
Pendulous abdomen
Malpresentation
Labor-
PROM chances increase
Cord prolapse
Slow cervical dilation
Prolonged/obstructed labour
Maternal and fetal injuries-
Injury at female genital tract
Asphyxia ,caput ect...
90. Immunologic disorders in pregnancy.
91. Placenta accreta
(causes, diagnostic, management).
The diagnosis of placenta accreta is made on a pathologic
specimen, obtained after hysterectomy. This definitive diagnosis is dependent
on the visualization of chorionic villi embedded in the myometrium with absence
of the decidual layer between them. The diagnosis of accreta can also be suggested by the use of sonography and
MRI
The other parts in number 141
92. Clinic signs of
eclampsia. Management and prevention. Findings at autopsy in
eclampsia patients.
Clinic signs of eclampsia
Many of the clinical manifestations of preeclampsia and
eclampsia can be explained on the basis of vasospasm.
Angiotensin Sensitivity
One of the earliest signs of developing preeclampsia is a
lowering of the effective pressor dose of infused angiotensin
II. In
normal pregnancy, the amount of angiotensin necessary to
increase the
diastolic pressure 20 mm Hg is increased, whereas in patients
destined
to develop pre-eclampsia the effective pressor dose is lower.
Weight Gain and Edema
Abnormal weight gain and edema occur early and reflect an
expansion of the extra vascular fluid compartment. This
expansion is
related to the increased capillary permeability that allows
fluid to
diffuse from the intravascular space with resultant expansion of
the
extracellular space.
Excessive weight gain and edema, especially if confined to the
lower extremities, do not establish a diagnosis of
pre-eclampsia.
Edema that includes the face and hands is of more concern but is
still
not diagnostic.
Elevation of Blood Pressure
The next sign usually detected is an elevation of blood
pressure,
particularly the diastolic pressure, which more closely mirrors
changes
in peripheral vascular resistance than does the systolic blood
pressure.
In the antepartum period, the blood pressure changes may occur
days
to weeks after the onset of pathologic fluid retention.
Proteinuria
Proteinuria completes the classic clinical triad of
pre-eclampsia.
In the antepartum period, this sign may occur days or weeks
after the
onset of hypertension. If the disease first manifests during
labor or in
the immediate postpartum period, this progression of events is
compressed into hours and sometimes minutes. The proteinuria of
preeclampsia/
eclampsia can be explained on the basis of afferent
arteriolar constriction with increased glomerular permeability
to
proteins.
Renal Function
It is usually only during the Stage of renal involvement,
clinically denoted by proteinuria, that detectable changes in
renal
function appear. The earliest change may be an increase in serum
uric
acid concentration. Creatinine clearance may decrease, and serum
creatinine and blood urea nitrogen levels may increase. The
hematocrit may also increase, reflecting a relative hypovolemia.
Renal
involvement may progress to significant oliguria and frank Tenal
failure.
Liver and Placental Function
In the liver, vasospasm may produce focal hemorrhages and
infarctions. Therefore, elevated serum enzyme levels are usually
present. Thrombocytopenia and
disseminated intravascular
coagulopathy may occur, reflecting an increased platelet
destruction
consistent with the HELLP syndrome. Spasm in the uteroplacental
vascular bed results in placental infarctions, which may become
extensive
and lead to a retroplacental hemorrhage. The indirect evidence
for
reduced uteroplacental blood flow is the increased incidence of
placental infarctions and intrauterine fetal growth restriction.
Central Nervous System Effects
Visual disturbances, such as blurred vision, spots, and
scotomata, represent degrees of retinal vasospasm. Increased
reflex
irritability or hyperreflexia aTe extremely worrisome signs of
central
nervous system (CNS) involvement and may connote imminent
seizures
related to cerebral vasospasm and hypoxia.
Management and prevention
The management of pre-eclampsia should begin at the first
sign
of abnormality, well before the diagnosis is confirmed. When
excessive weight gain or fluid retention is documented in the absence of other
pathognomonic changes, a brief dietary history should be
obtained to look for indiscretions and excesses. Appropriate
counseling should follow. The patient should be advised of
any concerns
and be requested to increase periods of bed rest, preferably
in
the left lateral position. For the following 48 hours,
activity out of bed
should be limited to eating meals (not preparing them) and
using the
bathroom. A no-added-salt diet may be prescribed. More
Severe
sodium restriction is contraindicated for all but those in
frank renal
failure. Follow-up is requested 48 hours or less later to
ton-firm
continued normal blood pressure and to determine the
efficacy of
treatment for the weight gain and fluid retention.
Successful treatment
dictates no further intervention, other than perhaps the
continuation of
the no-added-salt diet. If there has been no weight loss,
continued
reduction of activity with increased periods of bed rest and
more
frequent prenatal visits are indicated.
The treatment of hypertension depends to a great extent on
the
duration of the pregnancy and the elevation of blood
pressure. At the
lowest end of the hypertensive spectrum, 140/90 mm Hg, and
in
the absence of proteinuria, outpatient management is
possible.
Mild salt reduction (no added salt) and bed rest in the left
lateral
position are again advised. The patient and her family
should be
counseled regarding warning symptoms of deterioration.
Follow-up
should occur no later than 48 hours. Many patients in this
category
respond to bed rest with a normalization of blood pressure.
These
women merely require more frequent follow-up than usual.
For the nonresponders, the next step should be a trial of
bed rest
and a no-added-salt diet in the more controlled environment
of the
hospital. If blood pressure normalizes, observation should
be
continued for an additional 24 to 48 hours and the patient
should
follow a regimen of continued bed rest and diet with
frequent followup.
Nonresponders who are 37 weeks' gestation or greater should
be
evaluated for induction of labor. Those at less than 37
weeks' gestation
should continue bed rest and diet in the hospital for
several days while
undergoing the work-up detailed in Table. Patients with
continued
mild hypertension (not greater than 150/100 mm Hg) without
proteinuria and with normal laboratory values may be
considered for discharge and close follow-up.
93. Mechanism of labor
in occipito-posterior position.
94. Signs and
management of anterpartum asphyxia.
95. Ruptures of uterus.
Etiology and prevention.
96. Postdate pregnancy
and delayed labor.
Prolonged pregnancy is defined as pregnancy which
progresses beyond 42 weeks.[1]Prolonged pregnancy is associated with
fetal, neonatal and maternal complications. Risks increase after term and
significantly so after 41 weeks of pregnancy. A policy of induction of labour
appears to improve outcomes and reduce perinatal mortality.[2] Where
possible, first trimester ultrasound rather than last menstrual period (LMP)
dating should be relied on to assess pregnancy duration. This should be
determined using crown-rump measurement or head circumference if crown-rump
length is above 84 mm.[3]
Fetal
and neonatal risks
Prolonged pregnancy is associated with an increase in
perinatal morbidity and mortality. There is an increased risk of stillbirth and
neonatal death, as well as an increase in risk of death in the first year of
life. The increased mortality is thought to be due to factors such as
utero-placental insufficiency, meconium aspiration and intrauterine infection.
Fetal morbidity is also increased, with higher risks of:
·
Meconium aspiration.
·
Macrosomia and larger babies
resulting in:
·
Prolonged labour.
·
Cephalo-pelvic disproportion.
·
Shoulder dystocia.
·
Birth injury resulting in, for
example, brachial plexus damage or cerebral palsy.
·
Neonatal acidaemia.
·
Low five-minute Apgar scores.
·
Neonatal encephalopathy.
·
Neonatal seizures.
·
Features of intrauterine growth
restriction (IUGR) due to placental insufficiency
Maternal
risks
Prolonged pregnancy is also associated with increased risk
for the mother, including:
·
Obstructed labour
·
Perineal damage
·
Instrumental vaginal delivery
·
Caesarean section
·
Postpartum haemorrhage
·
Infection
Where labour is induced before the uterus or cervix are in
a favourable state, obstetric problems may follow which can have an adverse
effect on either mother or baby, including:
·
Need for caesarean section.
·
Prolonged labour.
·
Postpartum haemorrhage.
·
Traumatic delivery.
Epidemiology
·
The use of ultrasound in early
pregnancy for precise dating is thought to reduce the number of post-term
pregnancies compared to dating based on the LMP.[5]
·
Around 20% of pregnant women will
need induction of labour - the majority for post-term pregnancy.[6]
Risk factors[4]
·
Previous post-term pregnancy increases
the risk of recurrence in subsequent pregnancies.
·
Primigravidity.
·
High maternal BMI is associated with
longer gestation and increased rate of induction of labour.[7]Elevated
pre-pregnancy weight and maternal weight gain both increase the risk of a
post-term delivery.[8]
·
Genetic factors. There is an
increased risk of post-term pregnancy for mothers who were themselves born
post-term and twin studies also suggest a genetic role.
Presentation
Symptoms
·
When post-term, the neonate has lower
than normal amounts of subcutaneous fat and reduced mass of soft tissue.
·
The skin may be loose, flaky and dry.
·
Fingernails and toenails may be
longer than usual and stained yellow from meconium.
97. Pathologies of afterbirth
stage. Causes of placental separation.
98. Dyscoordinated
labor activity. Diagnostic, management.
Check question 151
99. Placenta previa.
Clinic, management.
Number 155
100. Prevention of
uterus’ ruptures.
Number 95
101. Primary powerless labor.
Diagnostic and management.
Primary uterine inertia occurs from
the early onset of labor and lasts during the its second stage until the end of
labor.
Primary uterine inertia is characterized by such
signs as:
Inadequate
uterine activity;
Lack of the
progressive cervical effacement and dilation;
Station of
presenting part in the pelvic inlet (- 3 station) for a long period of time and
slowly descent of the fetus in the case of “cephalopelvic disproportion”
absence;
Increased
duration of labor;
Maternal
exhaustion and impairment of fetal well-being .
Diagnosis of primary uterine inertia is made during dynamic
monitoring for woman during 2-3 hours. Important clinical evaluation of labor
duration is the rate of cervical dilation. If, the cervical dilation to 6 cm is
absent if from the onset of labor in nulliparous women have been passed 12
hours and in multiparous women have been passed 6 hours, the diagnosis of
primary uterine inertia has been made.
Management
of abnormal labor in the case of uterine inertia
Uterine
inertia, as a rule, accompanies by female sickness and tiredness. That’s
why for successful induction or augmentation of labor therapeutic rest should
be prescribed obligatory.
In the case of maternal exhaustion therapeutic rest should be
indicated. Obstetrics anesthesia is prescribed by combination of such drugs as:
Sol. Promedoli 1% - 1,0, Sol. Dimedroli – 2% -2, 0, Sol. Atropini
Sulfatis 0,1 % - 1,0. For this purpose Droperidoli 0,25 % - 1 ml or Natrii
Oxybuturatis 20 % should be prescribed also.
Induction of labor is the stimulation of uterine
contractions before the spontaneous onset of labor, with the goal of achieving
delivery.
Augmentation of labor is the stimulation of uterine
contractions that began spontaneously but are either too infrequent or too
weak, or both.
Stimulation
of labor is usually carried out with several ways:
intravenous administrated 5 units (1 ml)
oxytocin in 500 ml 0,9 % isotonic solution NaCl (dilute intravenous solution)
with the initiated dose 6-8 drops per minute to 40 drops per minute;
intravenous administrated 5 mg (1 ml)
prostaglandin F2a in 500 ml 0,9 %
isotonic solution NaCl with the initiated dose 6-8 drops per minute to 25-30
drops per minute;
combine intravenous administration of 2,5 units
of oxytocin and 2,5 mg of prostaglandin F2a in 500 ml 0,9 % isotonic solution
NaCl with the initiated dose 6-8 drops per minute to 40 drops per minute.
102. Tsovianov maneuver
at breech delivery.
103. Appendicitis and
pregnancy.
Diagnosis
The
most common presenting symptoms include anorexia, nausea, vomiting, and right
lower quadrant pain.[2,8,15] Fever and tachycardia may not be present during
pregnancy.[8,15] Right
upper quadrant pain, uterine contractions, dysuria, and diarrhea can also be
present.[1,3,6] It is believed that the appendix changes its
location during pregnancy with an upward displacement toward the costal margin
in the later stages of pregnancy (Figure 1).[16,17] Patients may then present with right upper quadrant
pain or entire right-sided pain, although the relocation of the appendix during
the later stages of pregnancy and right upper quadrant pain was not reproduced
in some patients.[1] A
presentation with right upper quadrant pain can be highly variable with an
incidence as high as 55%.[3]
Management and Treatment
Early
surgical intervention, with less than a 24-hour delay, has shown to be vital in
minimizing both maternal and fetal morbidity and mortality. Surgical delays of
more than 24 hours from the time of presentation have been associated with
appendiceal perforation and significant fetal loss and cases of maternal
mortality.[8,14] Various
tocolytic agents are used prophylactically for uterine irritability; however
their efficacy has not been demonstrated.[2,6]
Antibiotic
use during or after surgery may expose the developing fetus to potentially
teratogenic substances.[10] Pregnancy
related pharmacodynamic changes result in reduced maternal plasma levels of
antibiotics.[23] Gentamycin
and related aminoglycosides have been associated with nephrotoxicity and
ototoxicity, while tetracyclines may cause permanent tooth discoloration and
long bone malformation. Fluoroquinolones may cause dysplasia of cartilage and
arthropathies in children so are not currently recommended in pregnancy. If
perforation, peritonitis, or gangrenous appendix has occurred, broad-spectrum
antibiotics with anaerobic coverage such as the second-generation
cephalosporins would be appropriate.[12] Perioperative
(prophylactic) antibiotics were administered to 94% of the patients undergoing
appendectomies of which 60% were second-generation cephalosporins.[9] Ampicillin
or cephalosporins are used in combination with metronidazole in cases with
perforated or gangrenous appendix.[6]
104. Complications
after cesarean section.
· After cesarean section, the most common complications for the mother
are:
· Infection.
· Nausea, vomiting, and severeheadache after
the delivery (related to anesthesia and the abdominal procedure).
· Bowel problems, such asconstipation or when
theintestines stop
moving waste material normally (ileus).
· Injury during the delivery.
· Immature lungs and breathing problems, if the due date has been
miscalculated or the infant is delivered
before 39 weeks of gestation.3, 4
Long-term risks of cesarean section
Women who have a uterine cesarean scar have slightly higher long-term
risks. These risks, which increase with each additional cesarean delivery,
include:5
·
Breaking open of the incision scar during a
later pregnancy or labor (uterine rupture).
For more information, see the topic Vaginal Birth After Cesarean (VBAC).
·
Placenta accreta, placenta increta, placenta percreta (least
to most severe). These problems occur when the placenta grows deeper into the
uterine wall than normal, which can lead to severe bleeding after childbirth,
and sometimes may require a hysterectomy.
105. Clinically
contracted pelvis.
106. Contemporary
principles of management of gestosis.




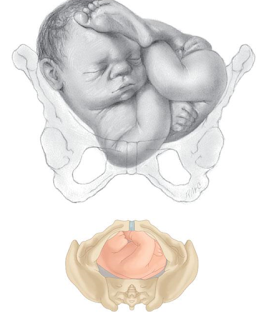

















































Thanks a lot.....we really appreciate...
ReplyDeleteThanks a lot.....we really appreciate...
ReplyDeleteNice One....
ReplyDeleteThanks
ReplyDeleteChemicals used in industries gives me Leukemia Cancer and it's all started when I wanted to get off my job to get another job that when I got diagnose, at that very point I was so scared to die because it has infected my blood cells also I was prescribed drugs like Cyclophosphamide,Busulfan,Bosutinib,Cytarabine, Cytosar-U (Cytarabine),Dasatinib in all that was just to keep me waiting for my dying day. I got inspired by what I read from a lady called Tara Omar on blog spot on how Dr Itua cure her HIV/Aids then they were lettered below that says he can cure Cancer so I pick his contact on the testimony she wrote then I emailed Dr Itua hopefully he replied swiftly to my mail then I purchased his Herbal medicine also it was shipped to me here in Texas, I went to pick it at post office so he instructs me on how the treatment will take me three weeks to cure my Leukemia Disease, Joyfully I was cured by this Dr Itua Herbal Medicine.
ReplyDeleteI will advise you too to give a try to Dr Itua Herbal Medicine with the following diseases that he can help you cure forever___Diabetes, Herpes,HIV/Aids, Bladder Cancer, Breast Cancer, Parkinson's disease,Schizophrenia,Lung Cancer,Breast Cancer,Colo-Rectal Cancer,Blood Cancer,Prostate Cancer,siva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity
Syndrome Fibrodysplasia Ossificans ProgresSclerosis,Seizures,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Copd,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,
Dementia.Vaginal Cancer, Kidney Cancer, Lung Cancer, Skin Cancer, Uterine Cancer, Prostate Cancer, Colo_Rectal Cancer, Leukemia Cancer, Hepatitis, Brain Tumors, Tach Disease,Love Spell, Infertility, Hpv. GoodLuck,XoXo****
Dr Itua Contact Information:::
Email (drituaherbalcenter@gmail.com)
WhatsApp-(+2348149277967)